Also known as Diabetes mellitus, Adult onset diabetes, Non-insulin dependent diabetes mellitus (NIDDM), Type 2 diabetes mellitus (T2DM), Hyperglycemia and High blood glucose
Overview
Type 2 diabetes is the most common type of diabetes in which the body fails to effectively use insulin. According to the WHO, more than 95% of people with diabetes worldwide suffer from type 2 diabetes. Until recently, type 2 diabetes was thought to be affecting only adults above the age of 40 years. However, due to stress and an inactive lifestyle, even people in their 20s are also at a high risk of diabetes.
Initially, Type 2 diabetes is mostly asymptomatic. Also, the symptoms tend to develop slowly and go unnoticed for a long time which makes it difficult to diagnose the condition. You might be at a higher risk of type 2 diabetes if anyone in your family has diabetes along with other risk factors such as obesity, inactive lifestyle, etc.
The gold standard test to diagnose type 2 diabetes is HbA1c as it gives you an idea of your blood glucose levels over the past 3 months. However, other tests such as fasting glucose and postprandial glucose tests are also commonly used. Once diagnosed, it is important to go for regular health check-ups and manage your diabetes properly because if left uncontrolled, it can impact other organs such as the kidneys, eyes, heart, nerves and legs.
Type 2 diabetes is managed with the help of diet control, exercise and use of oral medications. In cases of uncontrolled diabetes or high glucose levels, your doctor might recommend the use of insulin injections or pens.
Key Facts
Usually seen in
- Adults above 20 years of age
Gender affected
- Both men and women
Body part(s) involved
- Pancreas
- Eyes
- Nerves
- Feet
- Heart
- Kidneys
- Skin
- Reproductive system
Prevalence
- Worldwide: 462 million (2017)
Mimicking Conditions
- Metabolic syndrome
- Hypothyroidism
- Hemochromatosis
- Pancreatitis
- Cystic fibrosis
- Infections
- Cushing syndrome
Necessary health tests/imaging
- Glucose-random blood (RBG) test
- Glucose-fasting blood (FBG) test
- Glucose postprandial blood (PPBG) test
- Glycosylated hemoglobin (HbA1c) test
Treatment
- Biguanides: Metformin
- Sulphonylureas: Glimepiride & Glipizide
- Thiazolidinediones: Pioglitazone
- Meglitinides: Repaglinide & Nateglinide
- Alpha-glucosidase inhibitors: Acarbose & Miglitol
- DPP-4 inhibitors: Sitagliptin & Saxagliptin
- Incretin mimetics: Exenatide, Liraglutide & Dulaglutide
- Insulin: Lispro, Insulin Isophane & Glargine
Specialists to consult
- Endocrinologist
- Diabetologist
Related NGOs
- Home – DIYAbetes India
- Diabetes foundation India – DFI
- Diabetes care foundation of India
- Indian council for diabetic care | NGO
Symptoms Of Type 2 Diabetes
Type 2 diabetes is initially asymptomatic, which means it does not show symptoms for a long time. Moreover, it progresses at a very slow pace, which makes it difficult for any of the key warning signs to appear early. This is the reason why it is often said that NO symptoms are one of the most common symptoms of type 2 diabetes.
However, there are some symptoms that may indicate type 2 diabetes which include:
- Frequent urination
- Excessive thirst
- Increased hunger
- Unexplained weight loss
- Blurry eyesight
- Lack of energy/fatigue
- Delayed healing of cuts and other injuries
- Frequent yeast infections
- Numbness or tingling in the hands or feet
- Areas of darkened skin, usually affecting the armpits and neck
- Dry skin
Causes Of Type 2 Diabetes
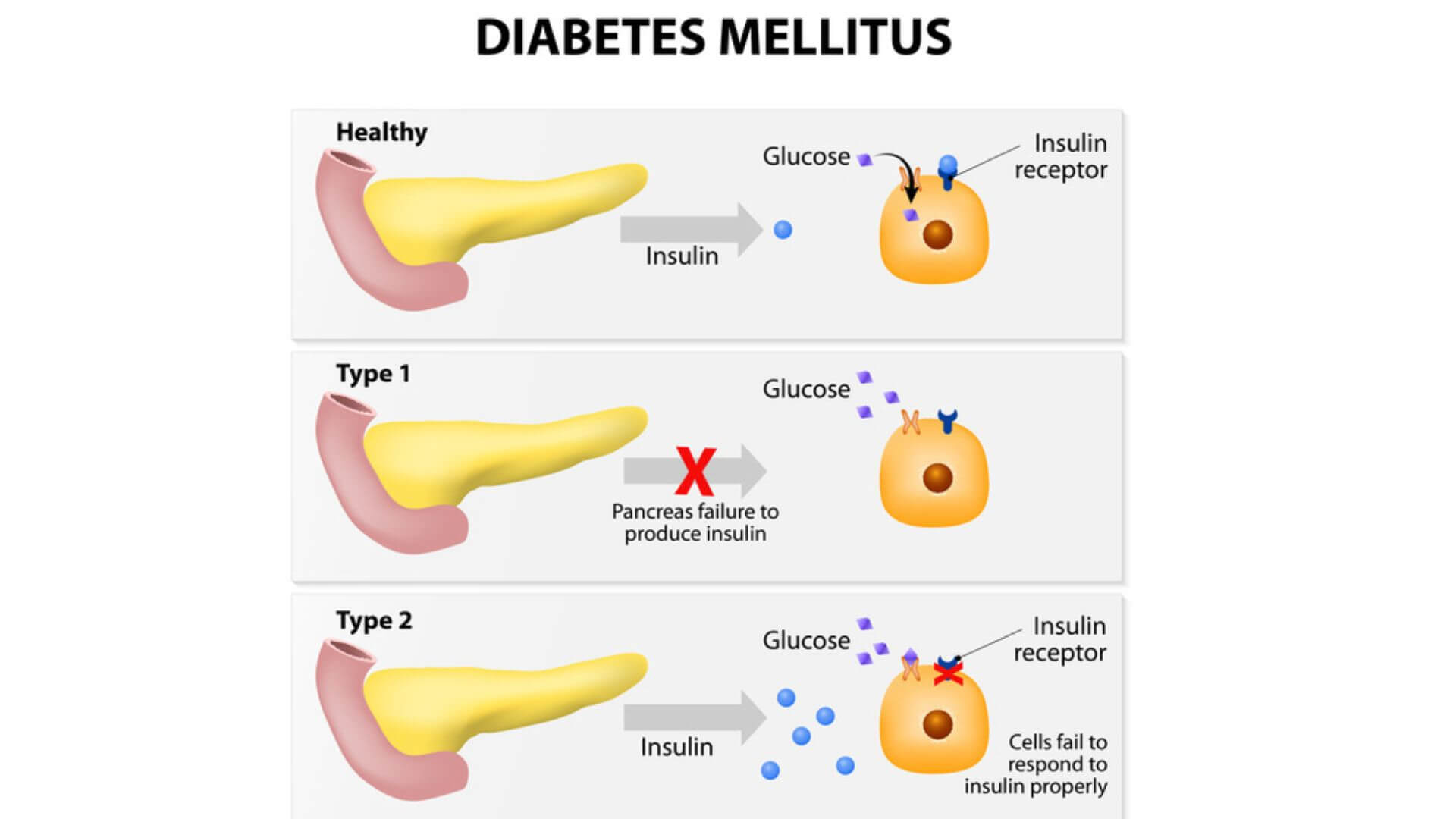
Insulin is a hormone produced by the pancreas. The pancreas is located below and behind the stomach. Insulin helps to move blood sugar (glucose) into the cells. Glucose is then stored inside the cells and later used for energy.
In type 2 diabetes, the body does not respond correctly to insulin. This is called insulin resistance. Thereby, blood glucose does not get into cells to be stored for energy. When glucose is not able to enter cells, a high level of glucose builds up in the blood. This is called hyperglycemia.
As blood glucose levels increase, the pancreas is triggered to release more insulin. Over a long time, the pancreas is not able to make enough insulin to meet the body’s demands. This leads to the symptoms of type 2 diabetes.
Risk Factors Of Type 2 Diabetes
The factors that increase the risk of type 2 diabetes are as follows:
Age: The risk of type 2 diabetes increases with age, especially after 45 years.
Family history: The risk of type 2 diabetes is higher in case parents or siblings have the condition. Also, genetic predisposition of high cholesterol, high blood pressure or cardiovascular disease can also predispose to type 2 diabetes.
Race and ethnicity: People of certain races and ethnicities like African American, Hispanic/Latino, American Indian, Asian American, or Pacific Islander are more likely to develop type 2 diabetes.
Unhealthy eating habits: Eating a calorie-dense diet with processed foods and beverages, and a diet low in whole, nutrient-rich foods, can significantly increase the risk of type 2 diabetes.
Being overweight or obese: Moreover, fat stored in the belly or abdomen region with waist circumference above 40 inches (101.6 centimeters) for a man or above 35 inches (88.9 centimeters) for a woman poses a higher risk of type 2 diabetes.
Sedentary lifestyle: Less physical activity can lead to weight gain and obesity thereby increasing the risk of diabetes.
Blood cholesterol levels: Low levels of high-density lipoprotein (HDL) cholesterol and high levels of triglycerides and low-density lipoprotein (LDL) can predispose to type 2 diabetes.
Prediabetes: In prediabetes, the blood sugar levels are higher than normal, but not high enough to be categorized as diabetes. If left untreated, prediabetes often leads to type 2 diabetes.
Pregnancy related issues: Gestational diabetes (diabetes during pregnancy) or giving birth to a child weighing more than 4 kgs increases the risk of type 2 diabetes.
Polycystic ovary syndrome (PCOS): PCOS which is characterized by irregular menstrual cycle, excessive facial hair growth and obesity also increases the risk of diabetes.
Smoking: The chemicals in cigarettes cause inflammation throughout the body. Additionally, when these chemicals react with oxygen in the body, they cause cell damage, called oxidative stress. Both oxidative stress and inflammation caused by smoking are related to increased risk of diabetes.
Sleep habits: Sleep disturbances can affect the body’s balance of insulin and blood sugar by increasing the demand on the pancreas thereby leading to diabetes.
Stress: Stress can stimulate the release of various hormones, which can predispose to high blood sugar levels.
Anxiety and depression: Psychological problems like depression are known to increase the risk of diabetes.
Diagnosis Of Type 2 Diabetes
The common lab tests include blood tests and urine tests. In addition to that, your doctor might conduct a thorough physical examination to check for signs of any skin problems. Also, imaging tests might also be advised in some cases to check the effect of diabetes on the nerves and other body organs. Psychiatric evaluation can also be recommended in people during the initial stages as most people tend to go through a rejection phase before finally accepting the fact that they have diabetes.
The commonly recommended blood tests used to diagnose diabetes include:
1. Random blood sugar test
The random blood glucose test is done to measure the levels of glucose circulating in the blood. This test is done to diagnose diabetes. You can take this test at any time of the day as it doesn’t need you to fast unlike other tests for diabetes. However, other tests are required to confirm the diagnosis. The test is done as a part of routine preventive health check-up or if you have symptoms of high blood glucose/hyperglycemia. Diabetes is confirmed, if your blood glucose levels are greater than or equal to 200 mg/dl.
2. Fasting plasma glucose test (FPGT)
This is one of the most common tests prescribed for diabetes. It is a blood test that measures the levels of glucose in the blood in the fasting state (empty stomach). Ideally, it is advised to not eat or drink anything (except water) for 8-12 hours before the test. It is the simplest as well as the fastest test to diagnose and monitor diabetes. If your blood glucose levels are greater than or equal to 126 mg/dl, diabetes is confirmed.
3. Postprandial blood glucose (PPBG) test
It is performed to measure glucose levels in the blood after a period of 2 hours from the start of the last meal. It is usually recommended to screen for prediabetes and also monitor treatment efficacy in patients undergoing treatment for diabetes. The test is usually recommended when the blood glucose level falls between 140 and 200 mg/dl.
4. Hemoglobin A1c (HbA1c) test
It is a blood test that measures a person’s average blood glucose level over the past 2 to 3 months. It is ideally used to check how well your diabetes is managed with medication. However, if your fasting and postprandial levels are high, then HbA1c is advised to confirm the diagnosis. HbA1c levels of 5.7% to 6.4% indicate prediabetes whereas levels higher than 6.5% indicate diabetes.
5. Other tests
If diagnosed with diabetes, you may need to undergo several health tests periodically to prevent complications and learn the effects of high glucose levels on other parts of the body. These include:
- Blood pressure
- Eye examination
- Foot examination
- Lipid profile
- Kidney function test (KFT)
- Liver function test (LFT)
- Vitamin B12 test
- Dental check-up
Celebs affected

Halle BerryThe Academy-award winning American actress Halle Berry was diagnosed with type 2 diabetes due to genetic predisposition but she makes sure to keep her diabetes under control.

Tom HanksOn the American Talk show “The Late Show” in the year 2013, Oscar winning Hollywood actor Tom Hanks had revealed that he was diagnosed with type 2 diabetes.
Prevention Of Type 2 Diabetes
With simple lifestyle changes such as diet control, staying active, keeping a tab on your weight and staying away from vices, you can lower your risk of type 2 diabetes. Here are a few tips to get started.
1. Make healthy food choices
- Taking care of your diet is one of the most essential components to manage and prevent diabetes.
- Switch to oils with high volume of monounsaturated fats & polyunsaturated fats like olive oil, canola oil, soybean oil or rice bran oil. Limit intake to one tablespoon a day.
- Restrict intake of foods that have a high glycemic index like white breads, white rice, fatty foods, and soda.
- Consume foods with low glycemic index like multigrain flour, whole grains, pulses, and non-starchy vegetables.
- Limit consumption of fast food.
Prevention Of Type 2 Diabetes

With simple lifestyle changes such as diet control, staying active, keeping a tab on your weight and staying away from vices, you can lower your risk of type 2 diabetes. Here are a few tips to get started.
1. Make healthy food choices
- Taking care of your diet is one of the most essential components to manage and prevent diabetes.
- Switch to oils with high volume of monounsaturated fats & polyunsaturated fats like olive oil, canola oil, soybean oil or rice bran oil. Limit intake to one tablespoon a day.
- Restrict intake of foods that have a high glycemic index like white breads, white rice, fatty foods, and soda.
- Consume foods with low glycemic index like multigrain flour, whole grains, pulses, and non-starchy vegetables.
- Limit consumption of fast food.
5 simple rules you must follow to keep your blood glucose level under control.
2. Watch your weight
- Lose weight to attain body mass index (BMI) between 18.5 and 24.9.
- Pay more attention to losing abdominal or belly fat as it can increase the risk of type 2 diabetes more than fat on any other part of the body like thighs, hips, and buttocks.
3. Exercise regularly
- Regular exercise can lower blood glucose and possibly reduce the amount of medication you need to treat diabetes, or even eliminate the need for medication.
- Even if you do not lose any weight, exercise can help keep type 2 diabetes under control.
- Start slowly with a low-impact exercise such as walking, swimming or jogging.
- Exercise at least three times a week for about 30 to 45 minutes.
- Warm up for 5 minutes before starting to exercise and cool down for 5 minutes after exercise.
- Be more active throughout the day. Avoid sitting for more than 2 hours at a stretch in a day.
- Parking your car far away, opting for stairs instead of the elevator or walking instead of sitting while talking on the phone can be handy tips to increase physical activity.
4. Manage stress better
- Stress can make blood sugar levels harder to control.
- It is very important to avoid unnecessary stress and indulge in activities that can help you relieve stress such as reading, traveling, sports, and other hobbies.
- Mind-body practices such as tai chi & yoga can help in managing stress and thereby preventing diabetes.
- You may join a yoga club nearby or dedicate 10-15 minutes every day for meditation.
Here are 6 amazing ways to battle chronic stress effectively.
5. Get a good quality sleep
- Make lifestyle changes to get sound sleep like going to bed and getting up at the same time every night and keeping electronics out of the bedroom.
- Sleep problems like sleep apnea can increase the risk of diabetes. If you have trouble sleeping, consult the doctor at the earliest.
6. Quit smoking
- Smoking has been found to directly increase the risk of several diabetes complications such as cardiovascular diseases, stroke, eye diseases, nerve damage, and kidney damage.
- It has also been found to reduce blood flow to the feet and other body extremities. This can lead to problems in feet and slow down the healing of injuries.
- Hence, it is wise to quit smoking to lower your risk of diabetic complications. Talk to your doctor for measures that can help you to quit smoking.
7. Drink in moderation
- Excessive drinking can cause unexpected spikes in blood glucose which can significantly affect your overall health, especially if you have diabetes.
- Men should consume no more than 2 drinks per day, and women no more than 1 drink per day. And in case you already are diabetic, alcohol can make it worse.
- Do not drink on an empty stomach.
Doctor To Visit
If you have been experiencing symptoms such as tingling sensation or numbness of the limbs, feeling excessively hungry or thirsty, or unexplained weight loss, then it is wise to consult following specialists:
- Endocrinologist
- Diabetologist
If you are already diagnosed with diabetes, then getting a regular health check-up is a must. This is because chronic or uncontrolled diabetes can impact other major organs of the body such as the eyes, legs, nerves, kidneys, and gums. So, if you suffer from any complications due to diabetes, then getting in touch with the respective specialist can help you to manage and prevent these problems. Some of the specialists who can help depending on the complication are:
- Nephrologist
- Neurologist
- Cardiologist
- Ophthalmologist
- Dentist
- Dietician
Consult India’s best doctor’s online with a single click. Click here to book an appointment.
Treatment Of Type 2 Diabetes
Diabetes can be treated with medications and injections along with few lifestyle modifications. Based on your blood glucose level, your doctor might recommend medicines/injections to control diabetes. Some of the common types of medicines for diabetes include:
A. Oral antidiabetics
1. Biguanides
This class of drug helps to improve glucose control by suppressing glucose production by the liver, decreasing the absorption of glucose by the intestine and increasing the insulin sensitivity. Metformin is the most commonly used biguanide to treat diabetes.
2. Sulphonylureas
These drugs are known to increase the secretion of insulin by the pancreas to manage diabetes. Some of the common examples of drugs belonging to this class include:
- Glimepiride
- Glipizide
3. Thiazolidinediones
This class of drugs help control diabetes by increasing insulin sensitivity in the muscles and fat tissues. Examples of this class of drug include:
- Pioglitazone
- Rosiglitazone
4. Meglitinides
They increase secretion of insulin by the pancreas to treat diabetes. Examples of this class of drugs include:
- Repaglinide
- Nateglinide
5. Alpha-glucosidase Inhibitors
As the name suggests, this class of drugs inhibit the enzyme alpha glucosidase thereby decreasing the absorption of glucose by the intestine. Some of the commonly available drugs under this class include:
- Acarbose
- Miglitol
6. DPP-4 Inhibitors
It works by improving the secretion of insulin by the pancreas thereby helping in the treatment of diabetes. Examples of this class of drugs are:
- Sitagliptin
- Vildagliptin
- Saxagliptin
7. Incretin mimetics
This class of oral antidiabetics are known to increase the secretion of the hormone insulin and help in controlling diabetes. Commonly known as glucagon-like peptide 1 (GLP-1) receptor agonists or GLP-1 analogues, this class includes drugs such as:
- Exenatide
- Liraglutide
- Dulaglutide
B. Injectables
This includes insulin (mainly human insulin) which increases the uptake of glucose by the cells and helps to control diabetes. There are 5 different types of insulin available currently which are recommended based on the severity of the condition. These include:
- Rapid-acting insulin (Examples: Lispro & glulisine)
- Short-acting insulin (Examples: Insulin regular & semilente)
- Intermediate-acting insulin (Examples: Lente & insulin isophane)
- Long-acting insulin (Examples: Ultralente & protamine zinc)
- Ultra long-acting insulin (Examples: Glargine, detemir & degludec)
Home-care For Type 2 Diabetes
A. Diet in diabetes
In the case of diabetes, it is essential to understand the concept of the glycemic index (GI). The glycemic index of a food refers to the effect the food has on the body’s blood sugar levels.
Foods are classified as low, medium, or high glycemic foods and ranked on a scale of 0–100. High GI is when the level is greater than 70, and low levels are less than 51. Diet in diabetes should include low GI foods whereas high GI foods should be avoided or limited. While choosing foods with a high GI, limit the portion size and pair them with sources of protein or healthy fat to reduce the impact on blood sugar.
Foods to prefer
1. Vegetables
Vegetables contain a good quantity of vitamins, minerals and are a great source of fiber. Green, leafy vegetables are full of essential vitamins, minerals, and nutrients. They’re also very low in digestible carbohydrates, so they won’t significantly affect blood sugar levels. Some of the examples of green leafy vegetables include spinach, avocados, cabbage, beans, broccoli, and kale.
2. Fruits
There is mixed perception about intake of fruits for diabetes. Some people believe that diabetics should completely cut down fruits from their diet while some think that one can include as much fruits as they want in their diet as it doesn’t have any impact on blood glucose level. However, neither is true. It is best to include fruits as an integral part of your daily meal plan while keeping a tab on the carbohydrate content.
Watch the video to know more about which fruits to eat and which fruits to avoid.
3. Protein-rich foods
Eating a protein rich diet can be very useful as proteins are more slowly broken down by the body than carbohydrates. They exert less effect on blood sugar level and hence can help to feel fuller for longer hours. Foods which are good sources of protein are fish, lean meats, and chicken.
4. Whole grains
Whole grains contain higher levels of fiber and nutrients than refined white grains. Consuming a diet rich in fiber is important for people with diabetes as it slows the process of digestion and therefore, helps keep blood sugar levels stable. A few examples of whole grains to be included in the diet are brown rice, quinoa, millet, buckwheat, and millet.
5. Seeds
Seeds like flax seeds and chia seeds are rich in fiber and low in digestible carbs. The fiber in seeds can lower blood sugar levels by slowing down the rate at which food moves through the gut. It also helps in maintaining glycemic management in people with diabetes.
6. Nuts
Nuts are a great source of fiber and vitamins and can be beneficial for regulating cholesterol. It has been proven regular consumption of nuts may reduce blood sugar levels. A few examples are walnuts, almonds, hazelnuts, and pistachios.
Foods to limit
1. Carbohydrate-rich foods
Carbohydrates are an important dietary part of all meals. However, people with diabetes are benefitted from limiting their carbohydrate intake in a balanced way. Replacing carbs with other alternative options or by pairing them with a healthy protein source are good options.
2. Saturated and trans fat
Saturated and trans fats in fried food and processed/packaged foods including chips, baked foods etc have been linked to a higher spike in blood glucose.
3. Alcohol
People with diabetes are generally advised to limit their alcohol intake to avoid sudden spikes in blood sugar levels.
4. Sugar-sweetened beverages
Sugar-sweetened beverages like soda, energy drinks, coffee, shakes & sweet tea lack important nutrients, and also contain a concentrated amount of sugar in each serving.
5. Excessive salt
Salt is not directly linked to blood glucose levels, but it is important to limit the amount of salt in case of diabetes management. People with diabetes are more likely to be affected by high blood pressure that is due to taking high salt in the diet, which increases the risk of heart disease, stroke, and kidney disease.
Dr. Beena Bansal (MBBS, MD, DM, Endocrinology) tells us about some simple ways to curb our food cravings. Watch the video now!
B. Exercise in diabetes
Aerobic activity is one of the effective exercise options to control diabetes. When done at moderate intensity it raises your heart rate and makes you sweat thereby helping you to maintain an optimum blood glucose level. Try brisk walking, light jogging, swimming or other aerobic exercises to maintain weight and control diabetes.
C. Regular health check-ups in diabetes
- Diabetes requires lifelong commitment towards following a healthy lifestyle, taking medicines on time and getting regular checkups to detect any complications.
- Check your blood sugar levels at home at least once a week.
- Get your HbA1c levels checked at least twice a year.
- In addition, make sure that your eyes, kidneys, heart and skin are in optimal health.
- Visit an eye specialist once a year to detect any signs of eye damage (diabetic retinopathy).
- Get your kidney function tests done at least 2 times a year.
- Inspect your feet regularly for any signs of numbness, pain or growth that may lead to ulceration and complications.
Complications Of Type 2 Diabetes
Insulin deficit, if left unchecked over the long term, can cause damage to many of the body’s organs, leading to disabling health complications such as:
Diabetes retinopathy: High blood glucose levels shall put you at an increased risk of eye problems such as blurred vision, cataract, and glaucoma.
Diabetic nephropathy: Excess glucose can cause thickening of blood vessels in the kidneys. This gradually impairs kidney function and increases the pressure on the kidneys and in the long run leads to chronic kidney failure and kidney failure.
Diabetic neuropathy: High blood glucose levels can affect the nerves by impairing the blood flow to the nerves by causing damage to the small blood vessels. This can result in tingling, numbness, pain or eventual loss of feeling that usually begins at the tips of the toes or fingers and gradually spreads upward. Damage to nerves of the heart can result in irregular heart beat. Nerve damage in the digestive system can cause problems with nausea, vomiting, diarrhea, or constipation.
Cardiovascular diseases: High blood glucose levels not only impairs the blood flow to the heart but can also increase the risk of atherosclerosis, which leads to narrowing of arterial walls throughout the body.
Diabetic ulcers: People with diabetes have an increased risk of developing foot ulcers. A diabetic ulcer is often painless, and people might not even know they have them. It is important to examine feet and legs regularly to identify diabetic ulcers and if needed, get prompt treatment.
Recurrent infections: High blood sugar can weaken the immune system. This may make one more susceptible to infections including bacterial and fungal infections.
Delayed healing: Cuts and blisters can become serious infections due to poor healing. Type 2 diabetes also causes poor circulation to the feet, which causes delayed healing of any cut or an infection. This can also lead to gangrene and loss of the foot or leg.
Hearing impairment: Hearing problems are more common in people with type 2 diabetes.
Sleep apnea: Obstructive sleep apnea is common in type 2 diabetes patients.
Dementia: Type 2 diabetes increases the risk of Alzheimer’s disease and other diseases that cause dementia.
Erectile dysfunction: In men suffering from diabetes, there is a high chance of developing erectile dysfunction around 10-15 years earlier than non-diabetics.
Alternative Therapies Of Type 2 Diabetes
Ayurveda
The science of Ayurveda manages diabetes through a combination of activities that include exercise (vyayam), dietary regulation (pathya), panchakarma (bio-purification) and medicines. It is best to consult an ayurveda consultant before taking any ayurvedic medicine for diabetes. Some household herbs and spices that you can include in your diet include:
- Powdered jamun seeds can be taken with water or buttermilk (chaach).
- Methi (fenugreek) seeds are taken with water 15-20 minutes before each meal. Methi has soluble fibers that slow down the digestion and absorption of glucose.
- Bael leaves are squeezed to prepare fresh juice that can be taken along with a pinch of black pepper.
- Dalchini (cinnamon) in powdered form can be taken with water as it helps in improving sugar as well as cholesterol level.
- Concentrated amla juice taken along with bitter gourd juice, helps in releasing more insulin.
- Karela (bitter gourd) juice is recommended to be taken every morning.
- Homeopathy
Defined as a complementary medicine, homeopathy majorly concentrates on improving the functioning of the pancreas to produce insulin. Homeopathy experts rely on the patient’s history and temperament to devise a constitutional medication. However, it is recommended to use the homeopathic medicines only if prescribed by the homeopath and that too alongside the usual course of medications suggested.
Yoga
It focuses on mindful exercise where a person’s attention is on the body or breathing and eases away worrying or depressing thoughts from the mind. Restorative yoga involves yoga poses and healing through relaxation techniques with conscious breathing and power yoga has been found to benefit for losing weight (a risk factor for diabetics). It has been studied for controlling both the symptom and complication associated with type 2 diabetes mellitus.
Acupuncture
This technique involves the insertion of very thin needles through the skin at strategic points of the body. Acupuncture may be effective in treating not only diabetes, but also in preventing and managing complications of the disease.
Living With Type 2 Diabetes
Learn more about the condition by reading about the condition and its complications online. In case of any doubt, get your queries answered by your expert. This includes knowing when to check blood glucose level, the lifestyle changes to follow, the type of glucometer to use, etc.
1. Know the highs and lows
Diabetes can put them at risk of various health problems right from obesity and heart disease to depression. Hence, learn to accept the fact and ensure you help patients to control blood glucose levels.
2. Go for appointments with the patient
This can help you to know what extra precautions to take and what changes you need to make to ensure the proper management of diabetes.
3. Follow the same diet pattern as the patient
This can not only make you more cautious when it comes to eating healthy but sharing the same fitness plan can help you to ease stress and stay healthy. Lifestyle changes become habits when done together. You can even get diet-related advice through e-consultation.
4. Talk to other caregivers and also let the patient connect with other diabetics
Sharing the experiences can make it easy to deal with diabetes and understand more about the condition. You can reach out to diabetes communities or online support groups for help.
References
- IDF DIABETES ATLAS. Ninth edition 2019. International Diabetes Federation (IDF)
- Understanding A1c Diagnosis. American Diabetes Association (ADA)
- Varma PP. Prevalence of chronic kidney disease in India – Where are we heading?. Indian J Nephrol. 2015;25(3):133-135.
- Kharroubi AT, Darwish HM. Diabetes mellitus: The epidemic of the century. World J Diabetes. 2015;6(6):850-867.
- Maiorino MI, Bellastella G, Esposito K. Diabetes and sexual dysfunction: current perspectives. Diabetes Metab Syndr Obes. 2014;7:95-105.
- Pandey A, Tripathi P, Pandey R, Srivatava R, Goswami S. Alternative therapies useful in the management of diabetes: A systematic review. J Pharm Bioallied Sci. 2011;3(4):504-512.
- Prediabetes – Your Chance to Prevent Type 2 Diabetes. Centers For Disease Control and Prevention (CDC). Last reviewed June 2020.
Did our information help you?In our relentless endeavour to keep improving our services, you are our eyes. Kindly take out sometime to guide us on how to serve your better.Share your feedbackSubscribe to stay informedSubscribe to our carefully crafted informative emailers by Medical Experts and be the first to get the latest health news, tips and important updates.Submit
DisclaimerRakesh Medicals ‘s sole intention is to ensure that its consumers get information that is expert-reviewed, accurate and trustworthy. However, the information contained herein should NOT be used as a substitute for the advice of a qualified physician. The information provided here is for informational purposes only. This may not cover all possible side effects, drug interactions or warnings or alerts. Please consult your doctor and discuss all your queries related to any disease or medicine. We intend to support, not replace, the doctor-patient relationship.